Nursing is a multifaceted profession that demands critical thinking, effective problem-solving, and a holistic understanding of the patient. Juggling diagnoses, medications, nursing interventions, and patient responses can feel overwhelming, especially for nursing students and newly graduated nurses. This is where the power of concept mapping comes into play.
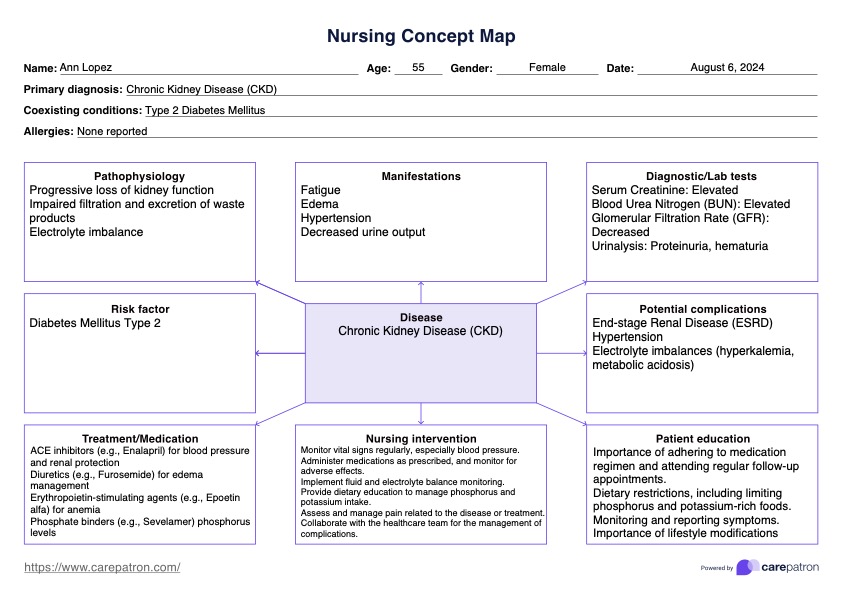
A concept map is a visual tool that allows nurses to organize and synthesize complex information, fostering deeper understanding and improved clinical decision-making. It connects key concepts, relationships, and critical information, providing a comprehensive picture of the patient’s condition and the care plan. This article will delve into the intricacies of nursing concept maps, explore their benefits, and provide detailed examples to illustrate their practical application in various clinical scenarios.
What is a Nursing Concept Map?
At its core, a concept map is a diagrammatic representation of knowledge. It uses nodes (shapes or boxes) to represent concepts and connecting lines to illustrate the relationships between those concepts. In nursing, these concepts might include:
- Patient Diagnoses: Medical and nursing diagnoses relevant to the patient’s condition.
- Signs and Symptoms: Observable or reported indicators of the patient’s health status.
- Pathophysiology: The underlying mechanisms of disease processes.
- Risk Factors: Elements that increase the patient’s susceptibility to health problems.
- Medications: Prescribed drugs, their mechanisms of action, and potential side effects.
- Nursing Interventions: Actions taken by the nurse to address patient needs and promote health.
- Patient Goals: Desired outcomes for the patient’s health and well-being.
- Evaluation: Assessing the effectiveness of interventions and making necessary adjustments.
The connecting lines, often adorned with action words or phrases, clarify the nature of the relationship between the concepts. For example, a line connecting "Hypertension" and "Sodium Intake" might be labeled "increased by," indicating that high sodium intake can contribute to hypertension.
Benefits of Using Nursing Concept Maps:
The use of concept maps offers several advantages for nursing professionals:
- Enhanced Critical Thinking: Concept maps encourage nurses to analyze information critically, identify patterns, and draw connections between seemingly disparate concepts. This process helps them develop a more comprehensive understanding of the patient’s condition.
- Improved Clinical Decision-Making: By visualizing the complex interplay of factors influencing a patient’s health, nurses can make more informed and effective decisions regarding diagnosis, treatment, and care planning.
- Enhanced Knowledge Retention: Actively constructing a concept map forces nurses to engage with the material in a meaningful way, leading to better retention and recall of information.
- Facilitated Communication: Concept maps can serve as a valuable communication tool for multidisciplinary teams, providing a clear and concise overview of the patient’s status and care plan. This promotes collaboration and ensures continuity of care.
- Improved Patient Education: Nurses can use concept maps to educate patients and their families about their condition, treatment options, and self-management strategies. The visual representation can make complex information more accessible and understandable.
- Effective Study Tool: Nursing students find concept maps to be an invaluable study tool for consolidating knowledge, preparing for exams, and understanding complex clinical scenarios.
- Holistic Patient Assessment: Concept maps encourage a holistic approach to patient assessment, considering not only the physical aspects of health but also the psychological, social, and environmental factors that influence well-being.
Types of Nursing Concept Maps:
While the basic principle remains the same, concept maps can be structured in various ways:
- Hierarchical Maps: Concepts are arranged in a hierarchical order, with the most general or overarching concepts at the top and more specific concepts branching out below. This structure is useful for organizing information based on levels of importance or generality.
- Spider Maps: A central concept is placed in the center of the map, with related concepts radiating outward like the legs of a spider. This structure is ideal for exploring the different aspects of a particular concept or problem.
- Flowchart Maps: Concepts are arranged in a sequential order, representing a process or sequence of events. This structure is useful for understanding the steps involved in a procedure or the progression of a disease.
- System Maps: Concepts are interconnected in a complex web, representing a system of interacting elements. This structure is suitable for analyzing complex systems, such as the human body or a healthcare organization.
Example 1: Congestive Heart Failure (CHF) Concept Map
This example illustrates a hierarchical concept map focusing on a patient with Congestive Heart Failure (CHF):
Central Concept: Congestive Heart Failure (CHF)
Branch 1: Etiology (Causes)
- Coronary Artery Disease (CAD) -> Leads to -> Myocardial Infarction (MI) -> Weakens Heart Muscle
- Hypertension -> Increases -> Afterload -> Strains Heart
- Valvular Heart Disease -> Impairs -> Blood Flow -> Causes Volume Overload
Branch 2: Pathophysiology
- Decreased Cardiac Output (CO) -> Activates -> Compensatory Mechanisms
- Increased Heart Rate (HR) -> Can Lead to -> Arrhythmias
- Increased Stroke Volume (SV) -> Initially Effective -> Eventually Fails
- Ventricular Remodeling -> Leads to -> Chamber Enlargement -> Worsens CO
- Fluid Retention -> Leads to -> Pulmonary Edema -> Causes -> Shortness of Breath (SOB)
- Sodium Retention -> Contributes to -> Edema
Branch 3: Signs and Symptoms
- Shortness of Breath (SOB) -> Especially -> Exertional Dyspnea & Orthopnea
- Edema -> Commonly in -> Lower Extremities
- Fatigue -> Due to -> Decreased CO
- Weight Gain -> Due to -> Fluid Retention
- Crackles in Lungs -> Indicates -> Pulmonary Edema
- Increased Heart Rate -> Compensatory Mechanism
Branch 4: Nursing Interventions
- Monitor Vital Signs -> Including -> Heart Rate, Blood Pressure, Respiratory Rate
- Assess Lung Sounds -> To Detect -> Pulmonary Edema
- Administer Medications -> Such as -> Diuretics, ACE Inhibitors, Beta Blockers
- Fluid Restriction -> To Reduce -> Fluid Overload
- Sodium Restriction -> To Minimize -> Fluid Retention
- Elevate Legs -> To Promote -> Venous Return
- Educate Patient -> About -> Medications, Diet, Lifestyle Modifications
Branch 5: Patient Goals
- Improved Breathing -> Decreased -> Shortness of Breath
- Reduced Edema -> Decreased -> Weight and Swelling
- Increased Activity Tolerance -> Able to -> Perform ADLs
- Adherence to Medication Regimen -> Take Medications -> As Prescribed
- Understanding of CHF -> Manage -> Condition Effectively
This concept map clearly illustrates the interconnectedness of the various aspects of CHF, from its causes and pathophysiology to its signs and symptoms, nursing interventions, and desired patient outcomes.
Example 2: Pneumonia Concept Map
This example utilizes a spider map approach to illustrate the different aspects of pneumonia:
Central Concept: Pneumonia
Spoke 1: Etiology
- Bacterial -> Streptococcus pneumoniae, Haemophilus influenzae
- Viral -> Influenza virus, Respiratory Syncytial Virus (RSV)
- Fungal -> Pneumocystis jirovecii (PCP)
- Aspiration -> Gastric Contents, Food
Spoke 2: Risk Factors
- Age -> Very Young & Elderly
- Chronic Illnesses -> COPD, Diabetes, Heart Failure
- Immunocompromised -> HIV/AIDS, Chemotherapy
- Smoking -> Damages -> Respiratory System
- Immobility -> Increases Risk of -> Aspiration
- Recent Surgery -> Weakened Immune System
Spoke 3: Pathophysiology
- Inflammation -> Of -> Alveoli
- Alveolar Filling -> With -> Fluid & Debris
- Impaired Gas Exchange -> Decreased -> Oxygenation
- Consolidation -> Of -> Lung Tissue
Spoke 4: Signs and Symptoms
- Cough -> Productive or Non-Productive
- Fever -> Elevated Body Temperature
- Chills -> Shaking and Trembling
- Shortness of Breath -> Dyspnea
- Chest Pain -> Pleuritic Pain
- Crackles/Rhonchi -> Abnormal Lung Sounds
- Sputum Production -> Color and Consistency Vary
Spoke 5: Nursing Interventions
- Administer Antibiotics/Antivirals -> As Prescribed
- Oxygen Therapy -> To Improve -> Oxygenation
- Monitor Respiratory Status -> Oxygen Saturation, Respiratory Rate
- Encourage Coughing and Deep Breathing -> To Clear -> Airways
- Position Patient -> To Promote -> Lung Expansion
- Hydration -> To Loosen -> Secretions
- Pain Management -> To Relieve -> Chest Pain
- Educate Patient -> On Infection Prevention, Medication Adherence
Spoke 6: Complications
- Sepsis -> Systemic Infection
- Respiratory Failure -> Inability to Maintain Adequate Gas Exchange
- Empyema -> Pus Accumulation in Pleural Space
- Lung Abscess -> Localized Infection in Lung Tissue
This spider map provides a comprehensive overview of pneumonia, encompassing its causes, risk factors, pathophysiology, signs and symptoms, nursing interventions, and potential complications.
Tips for Creating Effective Nursing Concept Maps:
- Start with a Central Concept: Clearly define the main topic or patient problem you want to explore.
- Identify Key Concepts: Brainstorm a list of relevant concepts related to the central concept.
- Organize the Concepts: Group similar concepts together and arrange them in a logical order.
- Draw Connecting Lines: Use lines to connect related concepts, indicating the nature of the relationship with action words or phrases.
- Keep it Concise: Use brief and clear language to describe the concepts and relationships.
- Use Colors and Symbols: Employ colors and symbols to highlight important information and enhance visual appeal.
- Review and Revise: Regularly review and revise your concept map as your understanding evolves.
Conclusion:
Nursing concept maps are powerful tools that can enhance critical thinking, improve clinical decision-making, and promote a deeper understanding of complex patient situations. By visually organizing and connecting key concepts, nurses can gain a holistic perspective of the patient’s condition and develop more effective care plans. Whether you are a nursing student or a seasoned professional, incorporating concept mapping into your practice can significantly improve your ability to provide safe, effective, and patient-centered care. The examples provided demonstrate the versatility of concept maps and their applicability to a wide range of clinical scenarios. By embracing this visual learning strategy, nurses can unravel the complexity of healthcare and provide the best possible care for their patients.