While the peak of the Zika virus epidemic may feel like a distant memory, the 2019 map of Zika virus transmission serves as a crucial reminder of the virus’s persistent presence and the ongoing risks it poses, particularly to pregnant women. Understanding the geographical distribution of Zika in 2019 allows us to analyze the factors contributing to its spread, assess the effectiveness of implemented control measures, and inform future prevention and response strategies.
This article will delve into the Zika virus map of 2019, examining the regions affected, the intensity of transmission, and the underlying causes for its prevalence in certain areas. We will also explore the implications of this distribution on public health, focusing on the vulnerable populations, the impact on healthcare systems, and the long-term consequences of Zika virus infection.
Understanding the Zika Virus
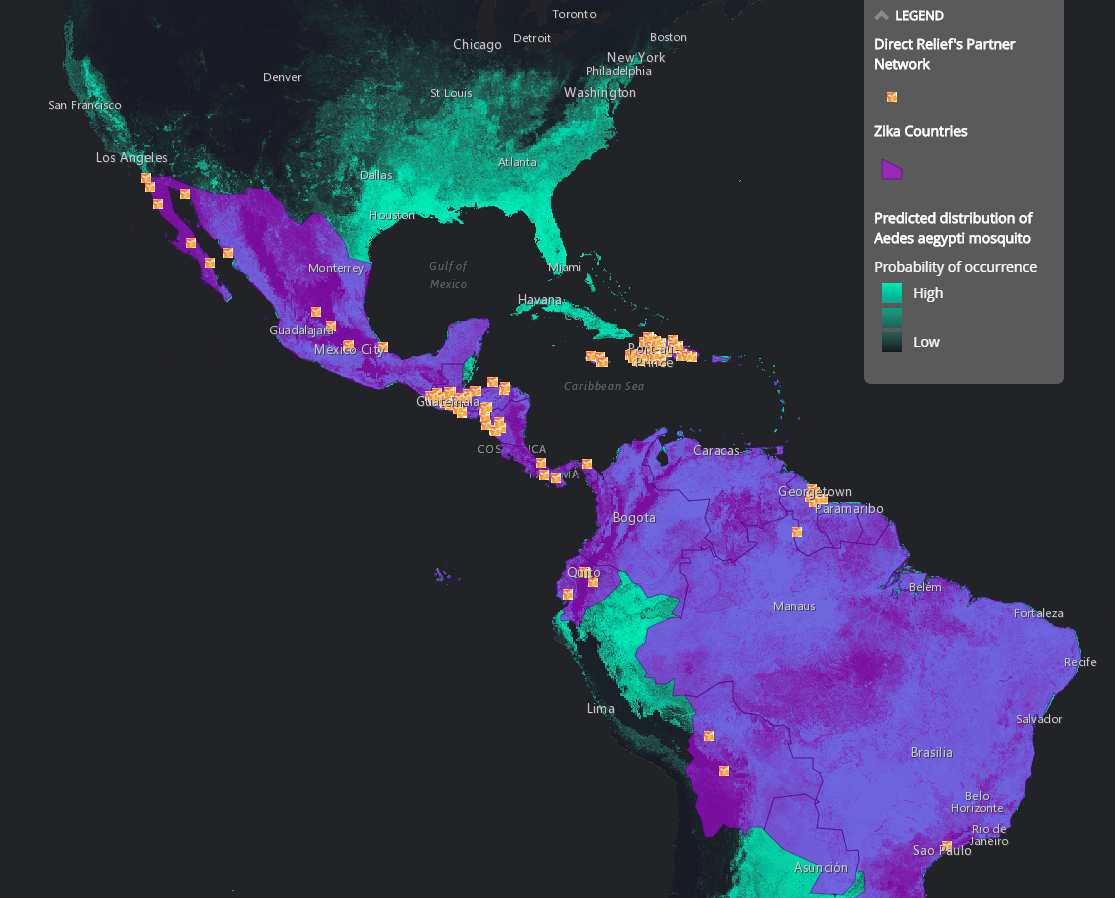
Before examining the 2019 map, it’s essential to understand the Zika virus itself. Zika is a mosquito-borne flavivirus, primarily transmitted by Aedes aegypti and Aedes albopictus mosquitoes. These mosquitoes are also responsible for spreading other diseases like dengue fever, chikungunya, and yellow fever, often leading to overlapping transmission patterns.
While Zika virus infection often presents with mild symptoms, such as fever, rash, joint pain, and conjunctivitis, its most significant concern lies in its potential impact on pregnant women. Zika infection during pregnancy can lead to serious birth defects, most notably microcephaly, a condition where a baby’s head is significantly smaller than expected, often accompanied by brain damage. Other congenital abnormalities associated with Zika virus infection include eye defects, hearing loss, and impaired growth.
Beyond congenital Zika syndrome, the virus can also cause Guillain-Barré syndrome (GBS), a rare autoimmune disorder that can lead to paralysis. While GBS is relatively uncommon, the association with Zika virus infection raises concerns for public health authorities.
Mapping Zika Virus: The 2019 Picture
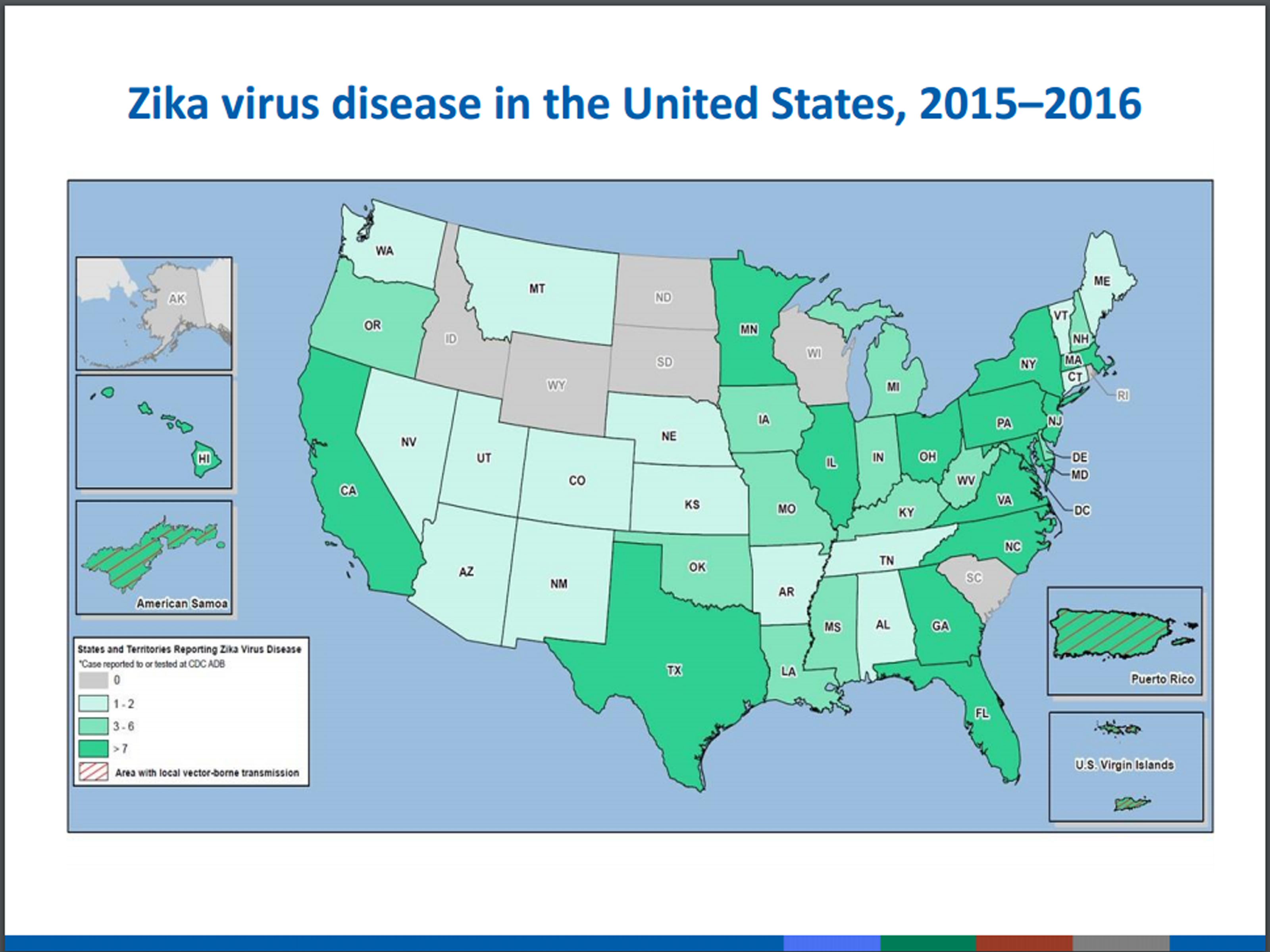
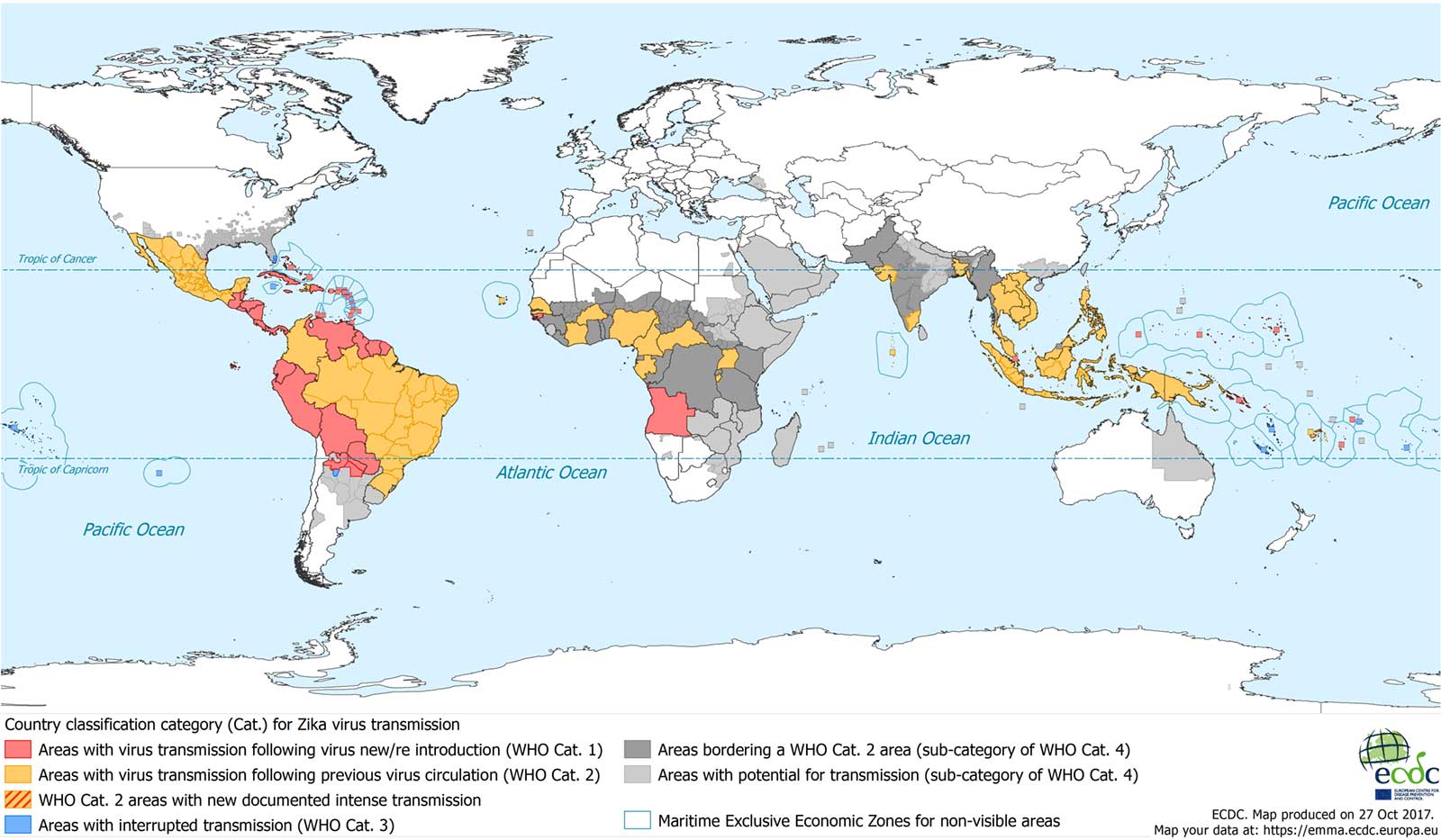
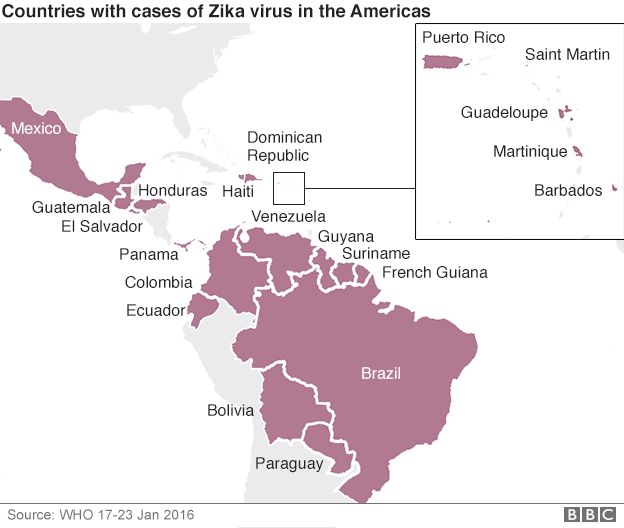
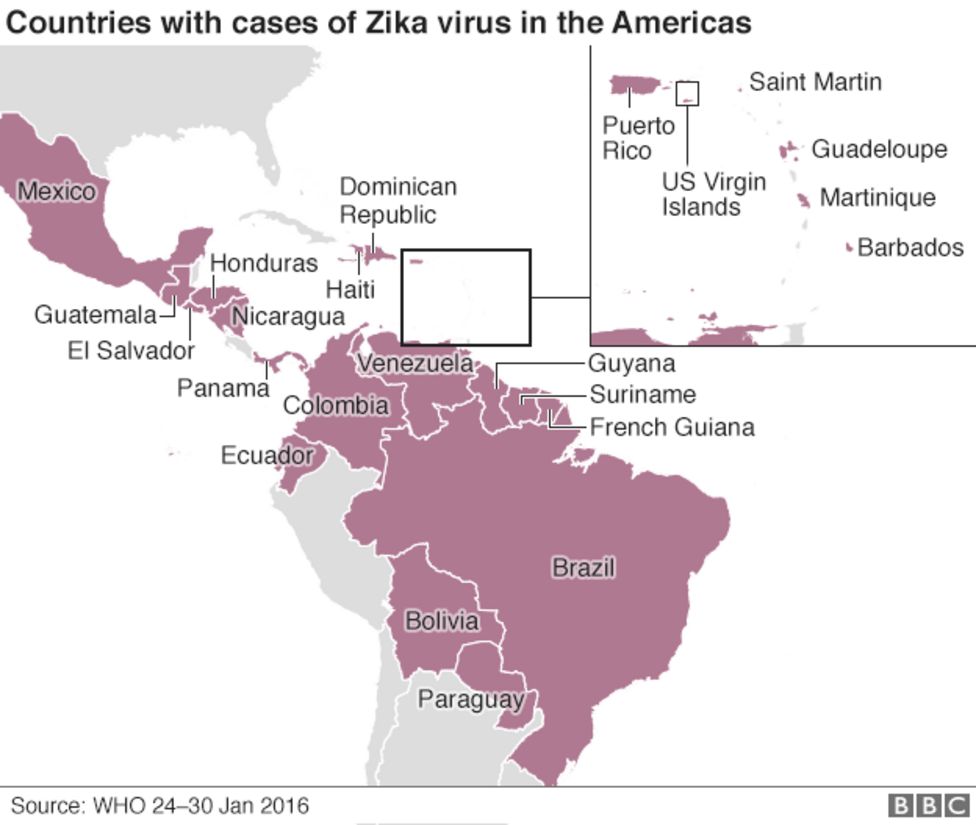
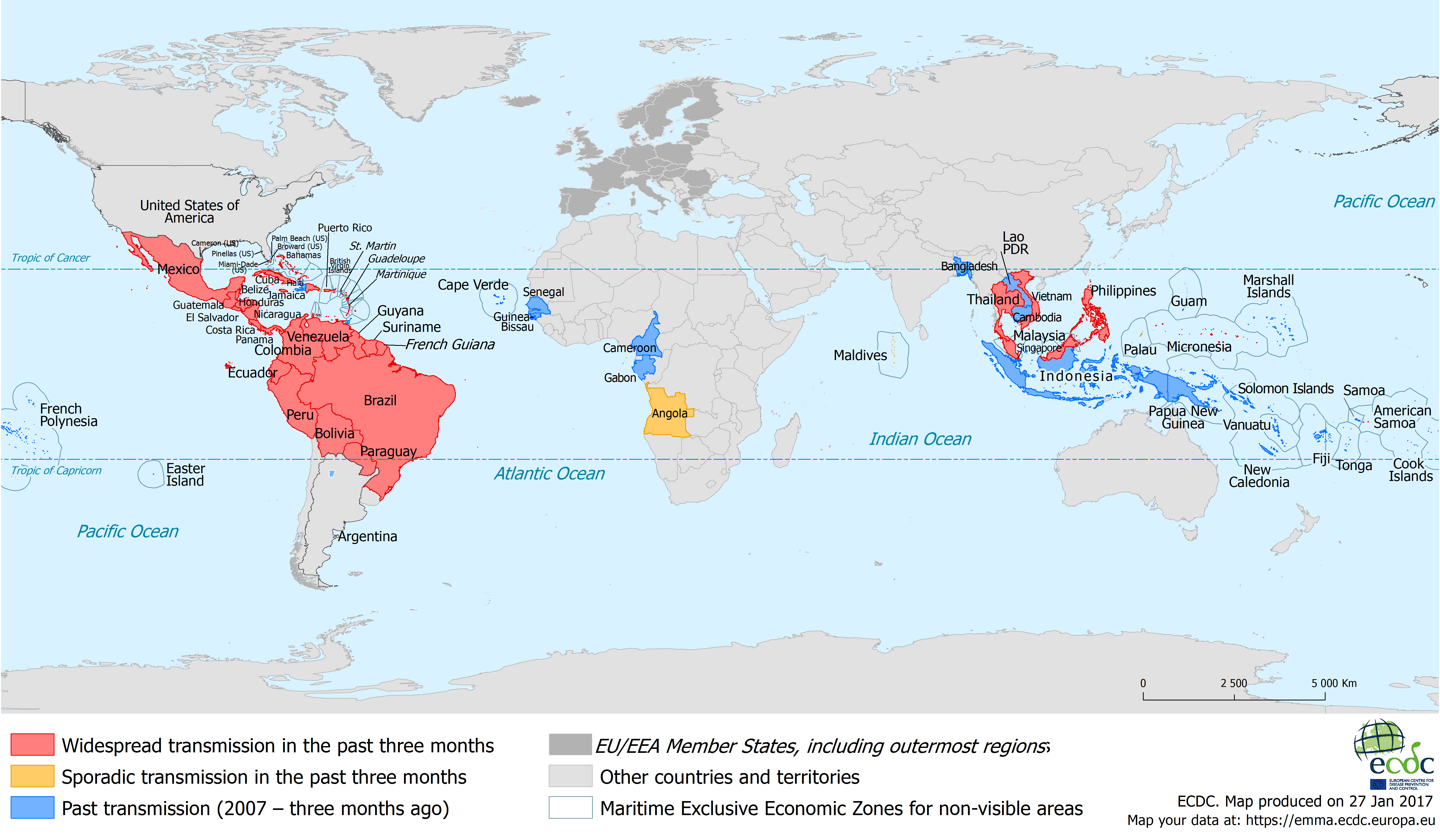
The 2019 Zika virus map, compiled from data provided by organizations like the World Health Organization (WHO), the Pan American Health Organization (PAHO), and the Centers for Disease Control and Prevention (CDC), reveals a complex and evolving landscape. While the global outbreak had subsided from its peak in 2016, the virus continued to circulate in several regions, primarily within the Americas, Southeast Asia, and Africa.
Key Regions Affected in 2019:
-
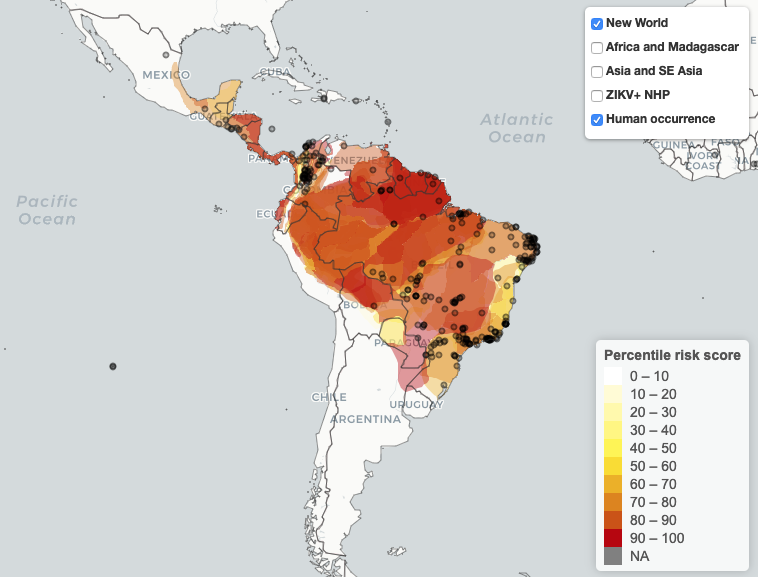
The Americas: The Americas remained a focal point for Zika virus transmission in 2019. While the number of reported cases significantly decreased compared to the peak of the outbreak, sustained transmission was observed in several countries, including Brazil, Colombia, Mexico, and parts of the Caribbean. The presence of the Aedes mosquito vector, coupled with favorable environmental conditions and ongoing travel, contributed to the continued circulation of the virus.
-
Southeast Asia: Several countries in Southeast Asia reported Zika virus cases in 2019, including Singapore, Thailand, Vietnam, and Malaysia. While the reported case numbers were generally lower compared to the Americas, the presence of the Aedes mosquito vector and dense populations created a conducive environment for transmission. Surveillance efforts and vector control measures played a crucial role in managing the spread of the virus in this region.
-
Africa: Zika virus has been known to circulate in Africa for decades. In 2019, several African countries reported Zika virus cases, although surveillance and reporting systems are often less robust than in other regions. Countries like Nigeria, Angola, and Ivory Coast reported sporadic cases, highlighting the potential for outbreaks in areas with limited resources and inadequate healthcare infrastructure.
Factors Influencing the 2019 Zika Virus Map:
Several factors contributed to the distribution and intensity of Zika virus transmission in 2019.
-
Vector Distribution: The presence and abundance of Aedes aegypti and Aedes albopictus mosquitoes are crucial determinants of Zika virus transmission. These mosquitoes thrive in tropical and subtropical climates and breed in stagnant water, making areas with poor sanitation and inadequate water management particularly vulnerable.
-
Climate and Environmental Conditions: Temperature, rainfall, and humidity play a significant role in mosquito breeding and virus replication. Warmer temperatures accelerate mosquito development and shorten the extrinsic incubation period of the virus, increasing the likelihood of transmission.
-
Population Density and Urbanization: Densely populated urban areas provide ample opportunities for mosquito breeding and human-mosquito contact, facilitating the spread of Zika virus. Rapid urbanization, often accompanied by inadequate infrastructure and sanitation, can further exacerbate the problem.
-
Travel and Migration: International travel and migration can introduce Zika virus into new areas, particularly when travelers become infected in endemic regions and then travel to areas with susceptible mosquito populations.
-
Surveillance and Reporting Systems: The accuracy and completeness of surveillance and reporting systems influence our understanding of Zika virus distribution. Countries with robust surveillance systems are more likely to detect and report cases, providing a more accurate picture of the virus’s prevalence.
-
Public Health Interventions: Vector control measures, such as insecticide spraying and the elimination of mosquito breeding sites, can significantly reduce mosquito populations and interrupt Zika virus transmission. Public health education campaigns promoting mosquito bite prevention and safe sex practices also play a crucial role in controlling the spread of the virus.
Implications of the 2019 Zika Virus Map:
The 2019 Zika virus map highlights several important implications for public health.
-
Risk to Pregnant Women: The primary concern associated with Zika virus infection remains the risk of congenital Zika syndrome in babies born to infected mothers. The continued circulation of Zika virus in 2019 underscored the importance of protecting pregnant women from mosquito bites and advising them to avoid travel to areas with ongoing Zika transmission.
-
Strain on Healthcare Systems: Managing Zika virus infection and its complications can place a significant strain on healthcare systems, particularly in resource-limited settings. Providing prenatal care, diagnostic testing, and specialized care for babies with congenital Zika syndrome requires substantial resources and trained healthcare professionals.
-
Long-Term Consequences: The long-term consequences of congenital Zika syndrome can be profound, affecting the physical and cognitive development of affected children. These children may require lifelong care and support, placing a burden on families and healthcare systems.
-
Economic Impact: Zika virus outbreaks can have a significant economic impact, particularly on tourism-dependent economies. Travel advisories and concerns about Zika virus infection can deter tourists from visiting affected areas, leading to economic losses.
-
Need for Continued Surveillance and Research: The 2019 Zika virus map underscores the importance of continued surveillance and research to monitor the virus’s distribution, understand its transmission dynamics, and develop effective prevention and treatment strategies. Research efforts should focus on developing a Zika virus vaccine, improving diagnostic tools, and developing interventions to mitigate the long-term effects of congenital Zika syndrome.
Conclusion:
The Zika virus map of 2019 serves as a valuable snapshot of the virus’s global distribution and the ongoing challenges associated with its control. While the peak of the outbreak may have passed, the virus continues to circulate in several regions, posing a persistent threat to pregnant women and public health. Understanding the factors influencing Zika virus transmission, implementing effective vector control measures, and providing comprehensive care for affected individuals are crucial steps in mitigating the impact of this virus. The lessons learned from the 2019 Zika virus map should inform future prevention and response strategies, ensuring that we are better prepared to address emerging infectious disease threats. Continued surveillance, research, and international collaboration are essential to protecting vulnerable populations and safeguarding global health security.